
American Nurses Foundation COVID-19 Two-Year Impact Assessment | American Nurses Foundation © 2022
Pulse on the Nation’s Nurses Survey Series:
COVID-19 Two-Year Impact Assessment Survey
Younger Nurses Disproportionally Impacted by Pandemic Compared to
Older Nurses; Intent to Leave and Staff Shortages Reach Critical Levels
March 1, 2022
America has suffered over 1 million deaths due to COVID-19 and the nation’s nurses continue to struggle through the
tragedy. As of this study, 60% of acute care nurses report feeling burned out, and 75% report feeling stressed, frustrated,
and exhausted, and for nurses under 35 the data is even more alarming. As a continuation of the Pulse on the Nation’s
Nurses Survey Series, and a one-year follow-up to the first annual impact survey conducted in Winter 2021, the American
Nurses Foundation has fielded another survey to probe today’s issues. The goal for the Two-Year Impact Assessment is to
identify the continued impact the pandemic has had on America’s nurses, with additional insight on the state of young
nurses, intent to leave, and staff shortages.
SURVEY BACKGROUND
The American Nurses Foundation and Joslin Insight launched a non-incentivized online survey to nurses across the United
States. The January 2022 survey was the second impact assessment survey conducted. The first was completed, or partially
completed, by 22,316 between January 19 - February 16, 2021. The recent Two-Year Impact Assessment was launched
between January 8-29, 2022. The survey was completed or partially completed by 12,694 nurses, with a ± 1.18% margin
of error at a 99% confidence level. More than 93% surveyed responded to all questions.
RESPONDENT PROFILE
The Foundation fielded this survey to nurses across
the entire continuum of care. Seventy-six percent of
respondents identified as White, 9% Black or African
American, 6% Hispanic or Latino, and 6% Asian. Thirty-
five percent indicated being 55 or older. Ninety-five
percent are currently employed, with 81% employed
full-time (data from retirees was not included). Fifty-
nine percent of respondents indicated their primary
work location is an acute care hospital, small to large;
11% primary, ambulatory, or outpatient care
facilities; and 6% community or public health
facilities. Seventy-seven percent of respondents
indicated they provide direct care to patients, and
90% have or may have had direct exposure to a COVID-19 positive patient.
Figure 1 – Respondent’s most recent place of employment, January 2022
American Nurses Foundation COVID-19 Two-Year Impact Assessment | American Nurses Foundation © 2022
YOUNG NURSES ARE LESS EMOTIONALLY HEALTHY & LESS OPTIMISTIC ABOUT THE FUTURE
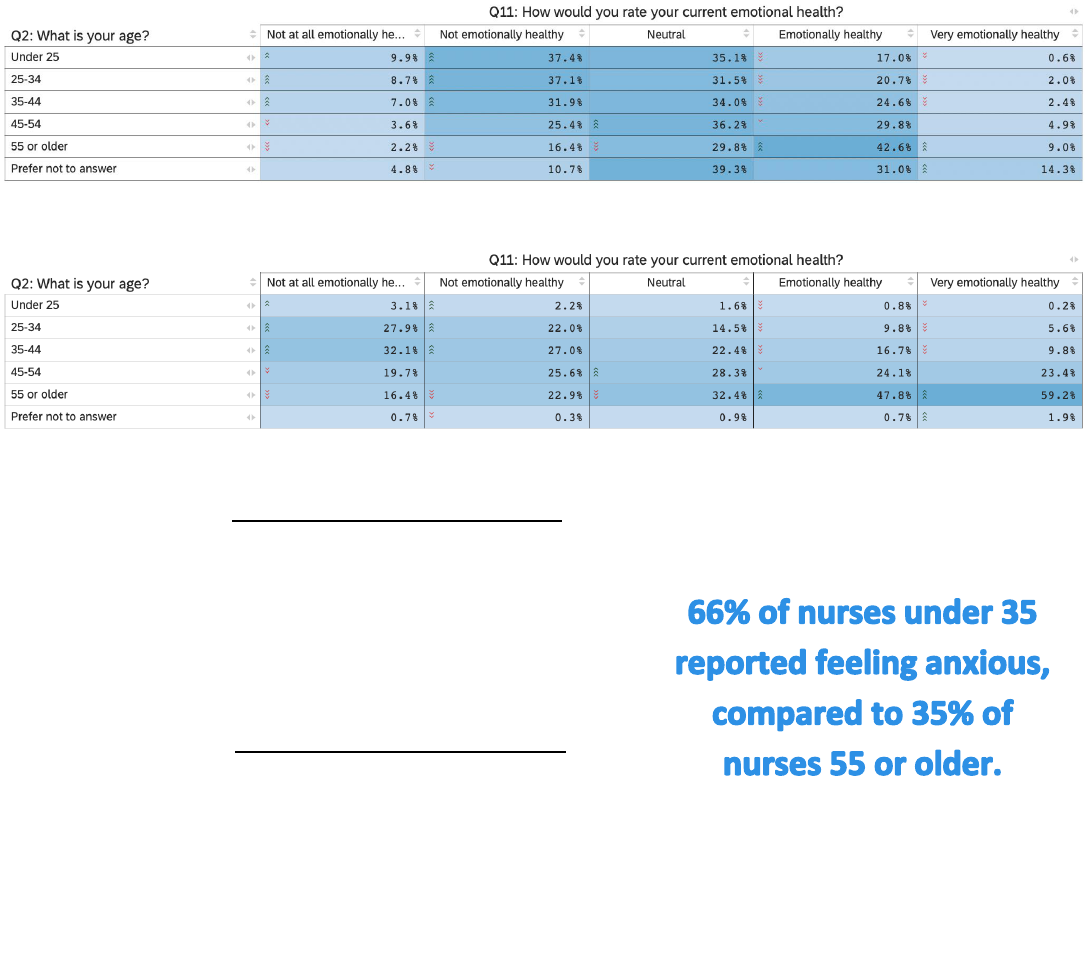
A statistically significant relationship exists between age and the emotional health of nurses. For all nurses, 30% said they
are ‘not emotionally healthy’ or ‘not at all emotionally healthy.’ For nurses under 25, that number is 46%, and for 55 or
older, 19% (Figure 2). Viewed differently, if one entered a room with one-hundred nurses who considered themselves
‘very emotionally healthy,’ fifty-nine would be 55 or older; six would be under 35 (Figure 3). This same trend applies to
years’ experience as a nurse. For nurses with less than 5 years’ experience, 40% are not or not at all emotionally healthy.
For nurses with more than 40 years experiences, it’s only 13%. Additionally, when younger nurses were asked to rate their
optimism between 0-10 based on everything they have experienced during the pandemic, with 0 being not at all optimistic,
the average was 5.00, compared to 3.77 for nurses under 35 and 5.89 for nurses 55 or older.
The results are consistent when analyzing the experience of feelings. For nurses under 35, 66% reported feeling anxious,
and 43% depressed, compared to 35% anxious and 21% depressed for nurses 55 or older. Perhaps of most concern when
considering the future of the nursing profession, two-out-of-three nurses under 35 reported feeling burned out, compared
to one-out-of-three nurses 55 or older.
Figure 2 - Relationship between age of nurse and current emotional health, by age brackets, January 2022
Figure 3 - Relationship between age of nurse and current emotional health, by emotional health categories, January 2022
By age, the following are not or not at all emotionally healthy:
• 47% Under 25
• 46% 25-34
• 39% 35-44
• 29% 45-54
• 19% 55 or older
By role, the following are not or not at all emotionally healthy:
• 46% Intensive or critical care nurses
• 46% Emergency department nurses
• 39% Medical-surgical nurses
• 38% Acute care (hospital) nurses
American Nurses Foundation COVID-19 Two-Year Impact Assessment | American Nurses Foundation © 2022
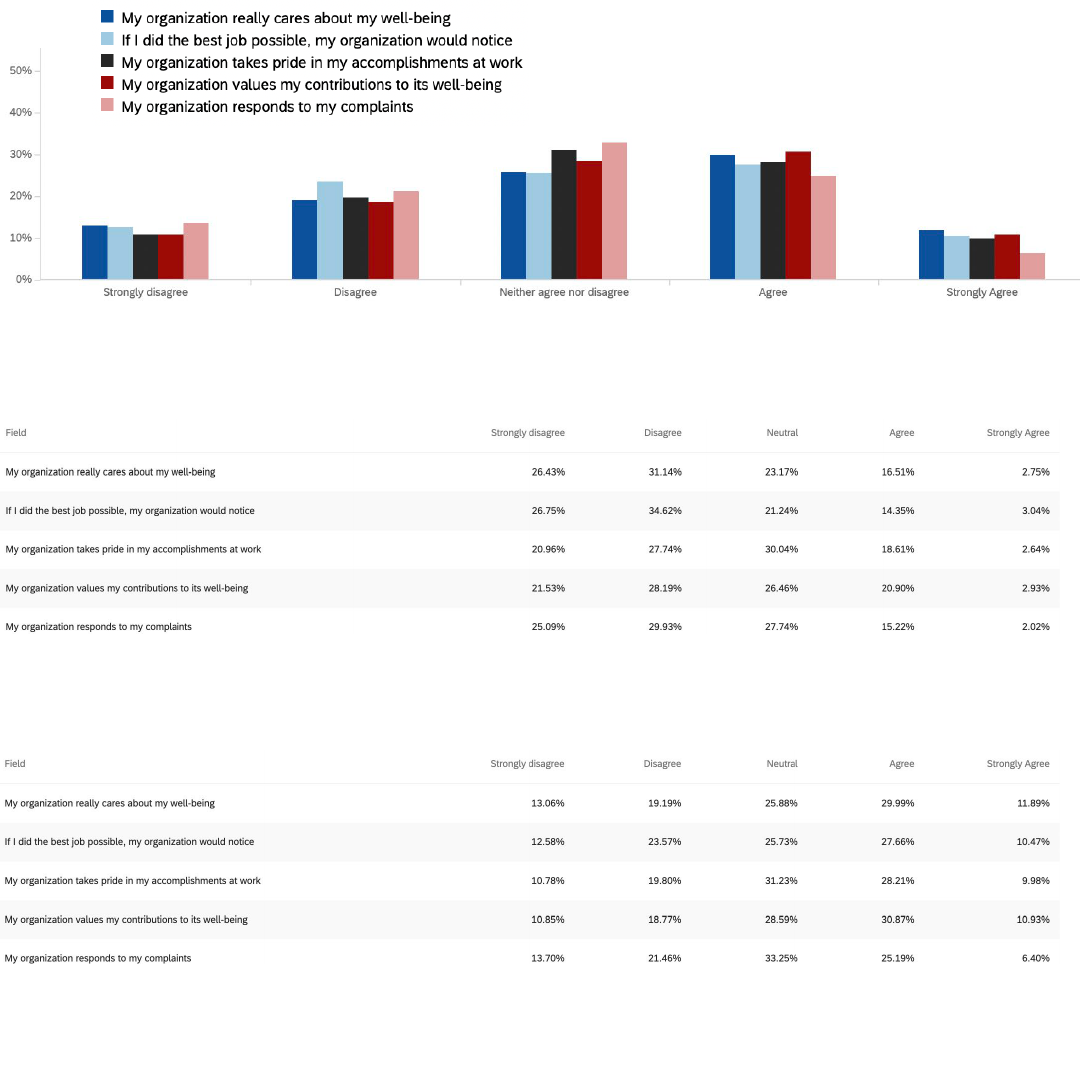
19% OF NURSES UNDER 35 FEEL THEIR ORGANIZATION CARES ABOUT THEIR WELL-BEING
In the Foundation’s third Mental Health and Wellness Survey conducted in September 2021, nurses were asked whether
they agree or disagree with certain statements concerning their Perceived Organizational Support. Scores were rated from
1-Strongly Disagree to 5-Strongly Agree. Over the past six months, the mean score across all questions has dropped
slightly, indicating a slight negative trend concerning nurses’ perception of support from their organizations.
While the decrease is of note, the gap of perceived organizational support between age groups is more critical. When
presented with the statement, ‘My organization really cares about my wellbeing,’ only 19% of nurses under 35 said they
‘agree’ or ‘strongly agree.’ By comparison, for nurses 55 or older, 42% said they agreed or strongly agreed. This gap is
consistent across other statements. For instance, to ‘If I did my best job possibly, my organization would notice,’ 61% of
nurses under 35 disagreed or strongly disagreed, compared to 36% of nurses 55 or older.
Figure 4 - Nurses respond to statements concerning perceived organizational support, January 2022
Breakdown of responses for age Under 35:
Figure 5 - Breakdown of responses to SPOS questions for nurses Under 35 years old, January 2022
Breakdown of responses for age 55 or older:
Figure 6 - - Breakdown of responses to SPOS questions for nurses 55 or older, January 2022
American Nurses Foundation COVID-19 Two-Year Impact Assessment | American Nurses Foundation © 2022
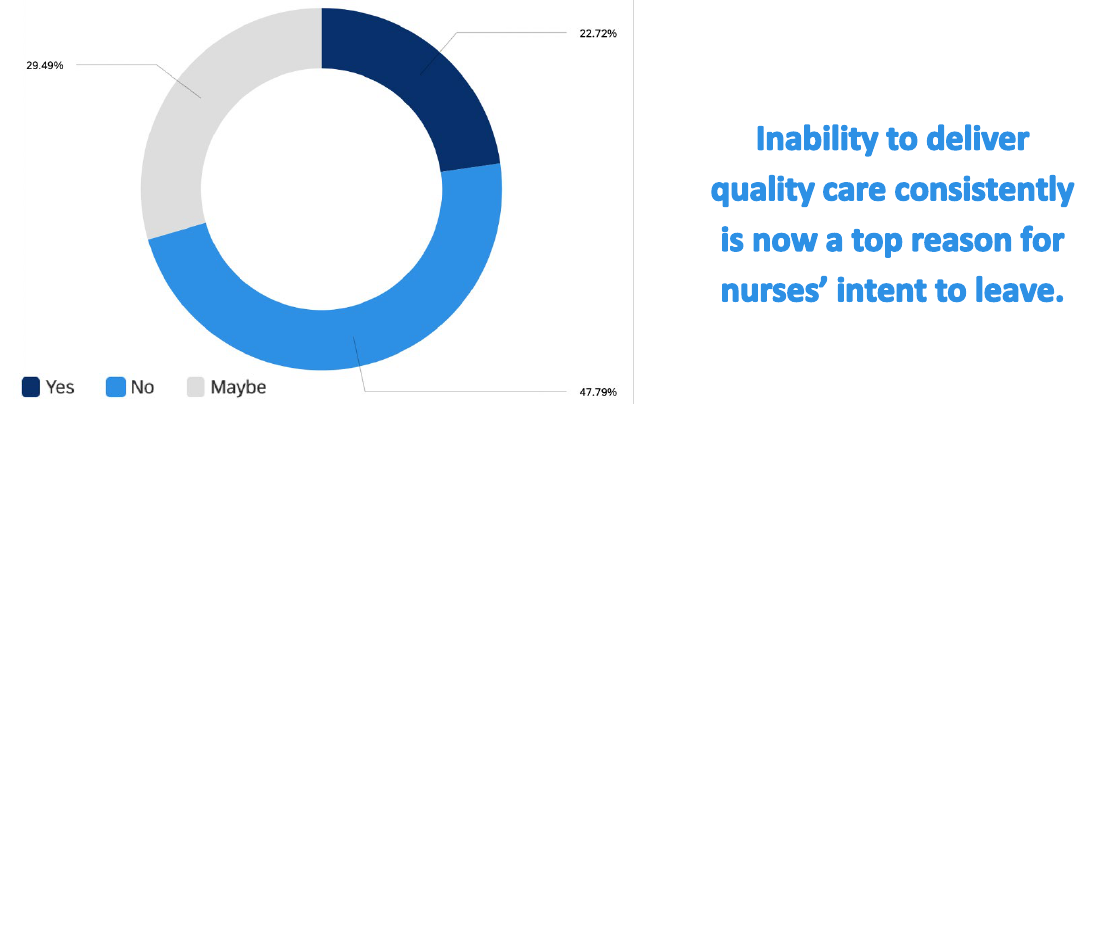
52% OF NURSES CONSIDERING LEAVING THEIR POSITION
One year ago, in the first annual impact assessment, 40% of nurses said they intended to leave or were considering leaving
their position. Today that has jumped by 30% with 52% of the nurses surveyed now intending to leave or considering
leaving. When analyzed by age, the issue is more concerning. In this survey, 63% of nurses under 35 said they intend to
leave or are considering leaving (31% Yes, 32% Maybe). For nurses 55 or older, who are already nearing retirement, 43%
said they intend to leave their positions or are considering leaving (18% Yes, 25% Maybe).
When nurses were asked why they want to leave, their top reasons were 1) insufficient staffing, and 2) work negatively
affecting health and wellbeing. Six months ago, in the third Mental Health and Wellness Survey, 41% of nurses indicated
insufficient staffing. That has increased 34% with 55% of nurses now identifying it as a reason for leaving. In terms of work
negatively affecting health and wellbeing, 51% of nurses identified this as their reason for leaving in this survey. In addition
to these, inability to deliver quality care consistently has emerged as an alarming reason. In September 2021, 25% of
nurses selected inability to deliver quality care as a reason for leaving. Six months later, that has jumped by 44% to 36%
of today’s nurses. Other reasons for wanting to leave are lack of support from their employer during the pandemic, distrust
of my employer, need for higher income, and poor organizational response to COVID.
Figure 7 - Nurses indicate whether they intend to leave their position in the next six months, January 2022
By age, the following intend to leave their position within the next 6 months:
• 37% Under 25
• 31% 25-34
• 27% 35-44
• 21% 45-54
• 18% 55 or older
By role, the following intend to leave their position within the next 6 months:
• 37% Telemetry nurse
• 32% Intensive, critical care nurse
• 31% Acute care (hospital) nurse
• 29% Emergency department nurse
• 27% Medical-surgical nurse
American Nurses Foundation COVID-19 Two-Year Impact Assessment | American Nurses Foundation © 2022
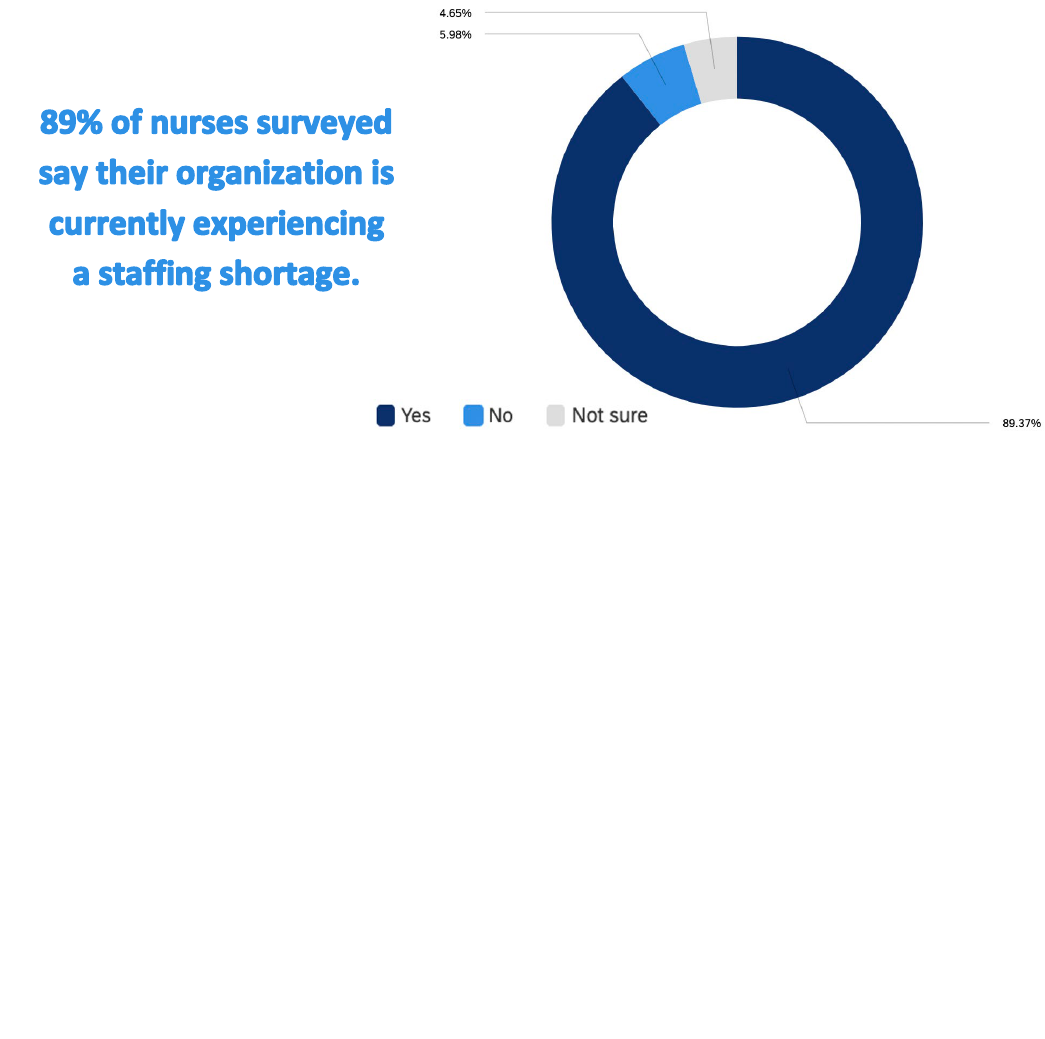
NINE-OUT-OF-TEN NURSES SAY THEIR ORGANIZATION IS UNDERSTAFFED
In this survey, nurses were asked whether their organization was experiencing a staffing shortage. Eighty-nine percent of
nurses indicated a shortage. Only 6% of nurses (predominately at schools of nursing) indicated no shortage. Of the nurses
who indicated a shortage, 54% said it was a ‘serious problem,’ and 40% said it was a ‘moderate problem.’ Less than half
of one percent said their organization’s staffing shortage was ‘not at all a problem.’ What is perhaps of most concern is
that this statistic no longer comes as a surprise. Information about organizations being short-staffed is widely accessible
and widely reported. The nursing profession is at the height of the nation’s workforce shortage.
By tracking data over the past two years, it has become evident that the nursing profession and health care delivery system
have entered a challenging time. Nurses leaving due to mental health concerns is a worrying truth for organizations.
Nurses leaving because of insufficient staffing signals a breakdown. If organizations are unable to stop the loss of
personnel, the problems have the potential to begin impacting patient care in dramatic ways.
Figure 8 - Nurses indicate whether their organization is experiencing a staffing shortage, January 2022
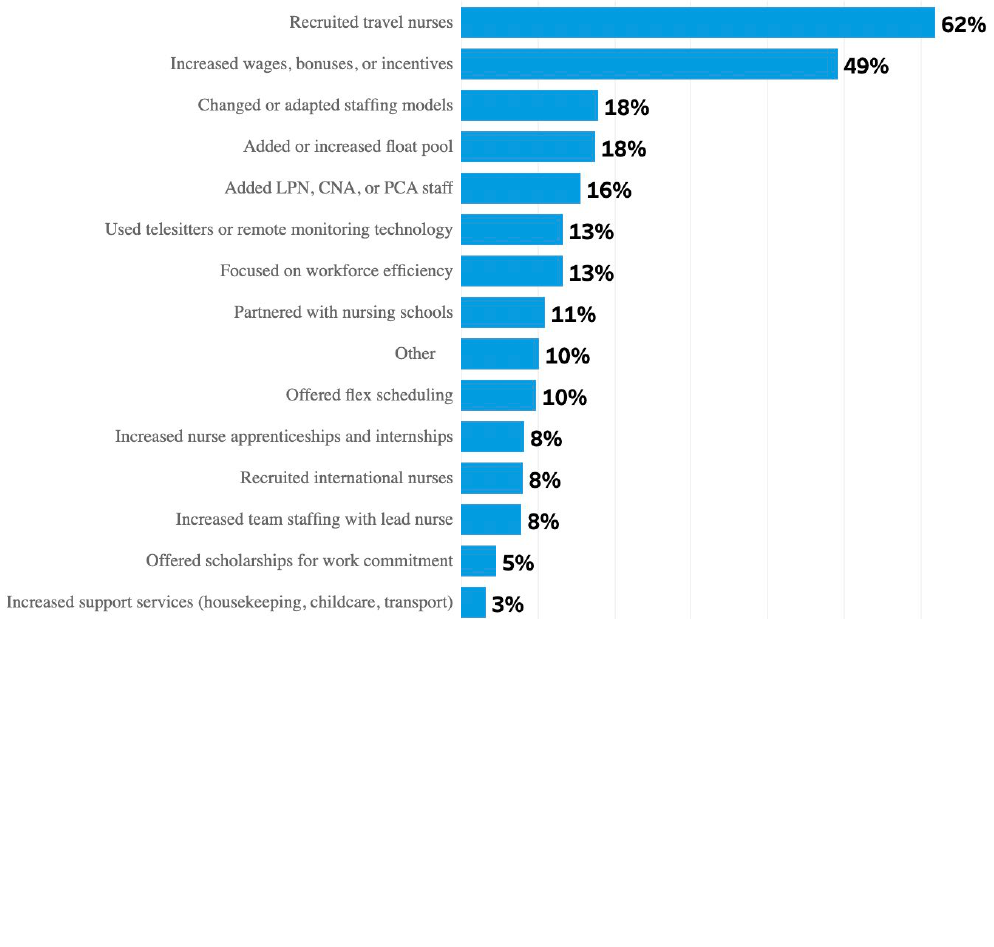
Facing these growing problems, many have wondered what options are available. In the survey, nurses identified solutions
to the shortage that have been implemented at their organization and have had a positive impact on work environment.
A hot topic, travel nurses were indicated by 62% of nurses as having had a positive impact. Another 49% indicated
‘increased wages, bonuses, or incentives.’ This was followed by ‘changed or adapted staffing models’ (18%), ‘added or
increased float pool’ (18%), and ‘added LPN, CNA, or PCA staff’ (16%). While salary received the second largest response,
it is necessary to view it in context.
When looking beyond fiscal solutions, other solutions are available. When asked what would improve work satisfaction, a
few other solutions stood out. In addition to increased pay, 52% of nurses surveyed selected ‘increase number of nurses
or support staff’ and 27% selected ‘support my work-life balance.’ Additionally, 15% selected ‘allow adequate time for
breaks’ and ‘enable me to take a day off when necessary.’ In the words of a pediatric nurse in San Diego, CA “If my
organization would just allow me to take my breaks and have lunch, I would be happy.”
American Nurses Foundation COVID-19 Two-Year Impact Assessment | American Nurses Foundation © 2022
ORGANIZATIONAL SOLUTIONS
The nursing profession has been under disproportionate stress due to the pandemic and typical hierarchical issues have
been heightened. When comparing the Two-Year Impact Assessment data to the August 2021 AONL COVID Impact
Longitudinal Study, a few items stand out.
i
In the AONL study, ‘adding or increasing float pool’ was identified as a solution
considered or implemented by 56% of nurse leaders to address shortages. This can be compared to 18% of nurses in the
two-year assessment who named adding or increasing float pool as a solution that has had a positive impact. Similarly,
42% of nurse leaders in the AONL study identified ‘flex scheduling’ as a possible solution, compared to 10% of nurses in
the assessment survey. The same applies to ‘increased support services,’ such as housekeeping and transportation. In the
AONL study, 17% of nurse leaders identified this as a solution, compared to 3% of nurses in this survey.
While no one-size-fits-all solution exists, this gap is significant and warrants attention. Nurse leaders are not to blame,
having been tasked with responding rapidly to an unprecedented challenge. As nurse leaders strive to address shortages,
these additional insights provide the needed information to help make data-driven decisions. Going forward, continued
critical thinking and creative discussions on these evidence-based needs of nurses may help identify solutions that can be
reasonably implemented by organizations. Ultimately, for a solution to be effective it must first be needed.
Figure 9 - Nurses identify solutions to the staffing shortage that have had a positive impact on work environment, January 2022
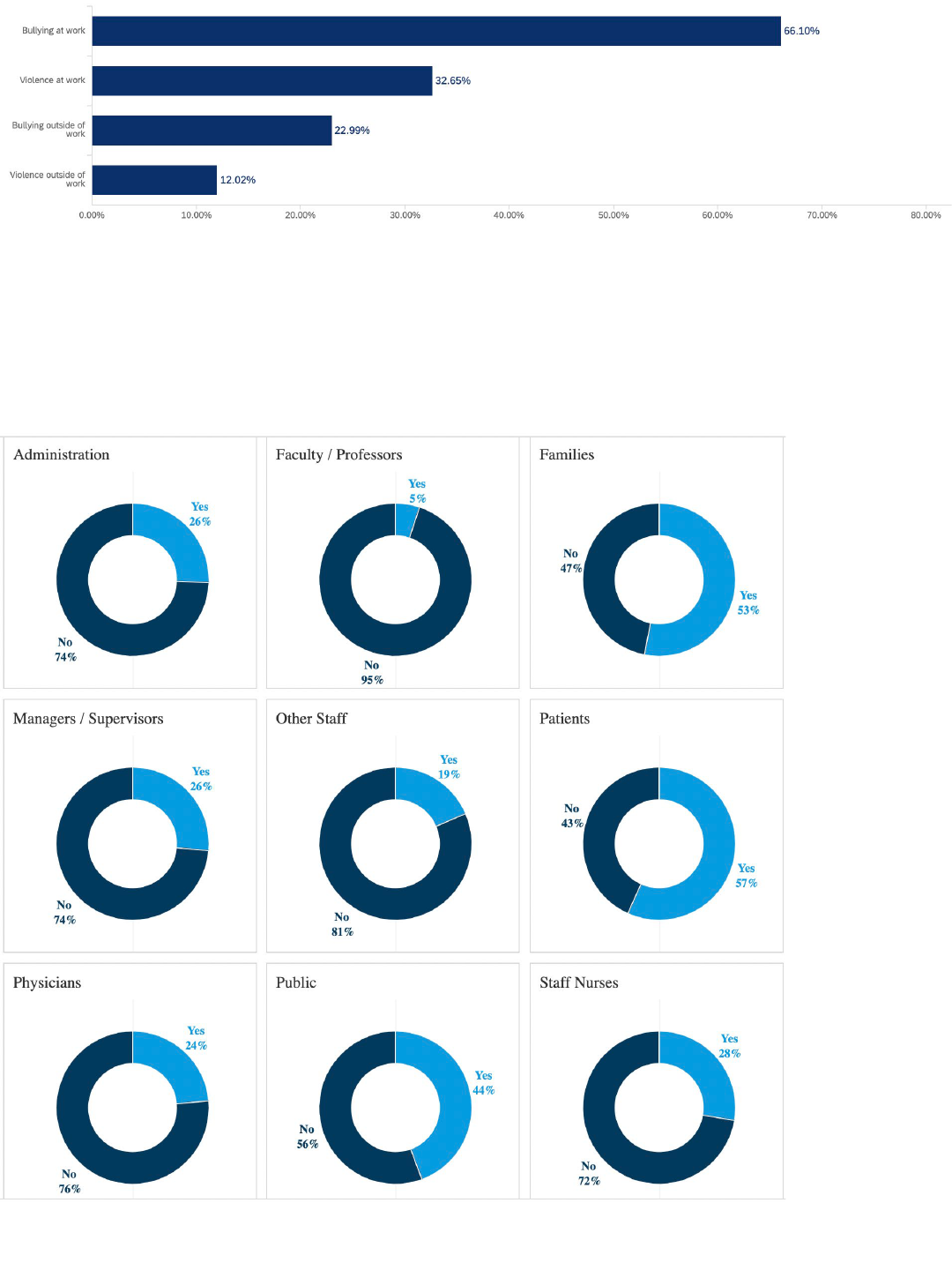
INCIVILITY & BULLYING HAS INCREASED DRAMATICALLY
A known and underreported reality for nurses is incivility and bullying. In this survey, nurses were asked if they have
experienced an increase in bullying and violence in the past year, at work and outside of work. Sixty-six percent of nurses
said they have experienced increased bullying at work. Thirty-three percent said they have experienced violence at work.
And the issue extends beyond the doors of the organization. An alarming 23% of nurses reported bullying outside of work,
and 12% reported violence outside of work. This is consistent with data gathered from the 2020 Healthy Nurse Survey.
ii
American Nurses Foundation COVID-19 Two-Year Impact Assessment | American Nurses Foundation © 2022
Figure 10 - Nurses identify whether they have experienced increased bullying or violence over the past year, January 2022
When analyzing bullying and violence by role, a significant number of those who reported an increase of bullying at work
were operating room and acute care hospital nurses. For violence at work, acute care, emergency department, intensive
or critical care, medical-surgical, and psychiatric and mental health nurses had significantly higher reporting. Incivility and
bullying were predominately identified as coming from patients and their families. Outside of work, bullying and violence
are being experienced by a significantly higher number of health policy, public health, and case management nurses.
Figure 11 - Nurses identify the source of incivility and bullying at work, January 2022
American Nurses Foundation COVID-19 Two-Year Impact Assessment | American Nurses Foundation © 2022
ACCEPTANCE, THEN RENEWAL
These are challenging and uncertain times for the nursing profession and the entire health care delivery system. Most of
America’s nurses feel stressed, frustrated, and exhausted. Feelings of motivation, empowerment, and confidence have
dropped in the past six months. Reports of feeling happy have dropped by one-third, and reports of feeling betrayed,
undervalued, and unsupported have risen. With hope and optimism also deteriorating, and 60% of acute care nurses now
reporting burn out, there is no doubt that hospitals and health care facilities are facing extraordinary workforce challenges
and a difficult future.
Magnifying mental health issues, the nation’s labor shortage has been felt acutely in health care. As of this study, 89% of
nurses have reported staffing shortages at their organization, with more than half saying their shortage is a serious
problem. Since March 2020, nurses have been isolated, delivering care behind layers of personal protective equipment.
As expressed in interviews, feeling alone was already a norm for many nurses, especially novice nurses when introduced
to bedside care. But the pandemic and growing shortages have amplified their sense of isolation and doubt, and nurses’
scores of Perceived Organizational Support indicate that many do not feel supported by their organizations.
Of all the industries impacted by COVID, few would argue that the profession of nursing has not taken the brunt of the
burden. Given everything nurses have been through since the World Health Organization officially declared COVID-19 a
pandemic, it comes as no surprise that nurses are seeking other opportunities. Quantitatively, intent to leave is on the
rise. Over half of America’s nurses plan to leave or are considering leaving their position in the next six months. If intent
becomes action, organizations will encounter more difficult times ahead.
While the pandemic has impacted many across the continuum of care, a disproportionate number of younger and novice
nurses are struggling, especially in acute care, emergency department, critical care, and medical-surgical roles. Younger
nurses in these roles are exposed to the pandemic’s worst and their mental health is failing as result. In this survey, 66%
of nurses under 35 reported feeling anxious and 47% depressed. Furthermore, 60% of nurses under 35 have experienced
an extremely stressful, violent, or traumatic event due to COVID-19, and should undergo further evaluation for potential
post-traumatic stress. Much may be attributed to younger and novice nurses’ proximity to the bedside, with 46% of acute
care nurses reporting not being emotionally healthy. That the pandemic has disproportionately impacted younger nurses
is a fact supported by strong data. But the problem is not that nurses 55 or older or with many years of experience report
stronger emotional health; the problem is that younger and novice nurses feel they are not being heard.
Ultimately, change requires acceptance. Acceptance that the last two years have been an emotional journey for the entire
world, for the nation, and for communities and families. Acceptance that the last two years have taken a toll on the health
care delivery system and that the weight of the world has rested on the shoulders of health care professionals. With the
data behind the problem no longer coming as a surprise, it is time to assess the damage and begin the important work of
renewal. The goal now is for policymakers, professional organizations, health systems, and leadership to act. The journey
will be made easier when all healthcare professionals come together with unified direction. There is no perfect one-size-
fits-all solution to solve all of today’s problems, but there are imperfect solutions that can provide relief and mark the
beginning of much needed change.
To
this end, the American Nurses Foundation and the American Nurses Association have launched initiatives to address
the mental health and well-being of nurses. Some available programs that are providing relief include the
Well-Being
Initiative and the Coronavirus Response Fund for Nurses. But these new survey findings show that gaps remain that still
need to be addressed. Moving forward, the goal is to drive a coordinated and robust approach that supports nurses as
they continue to provide patient care during unprecedented and challenging times.

American Nurses Foundation COVID-19 Two-Year Impact Assessment | American Nurses Foundation © 2022
i
“COVID-19 Impact Longitudinal Study.” American Organization for Nursing Leadership and Joslin Insight, August 2021.
https://www.aonl.org/resources/nursing-leadership-covid-19-survey
ii
“Healthy Nurse Healthy Nation Year Three Highlights 2019-2020.” American Nurse, September 2020.
https://www.myamericannurse.com/healthy-nurse-healthy-nation-year-three-highlights-2019-2020/
